Make sure the tape measure is straight when you go around.
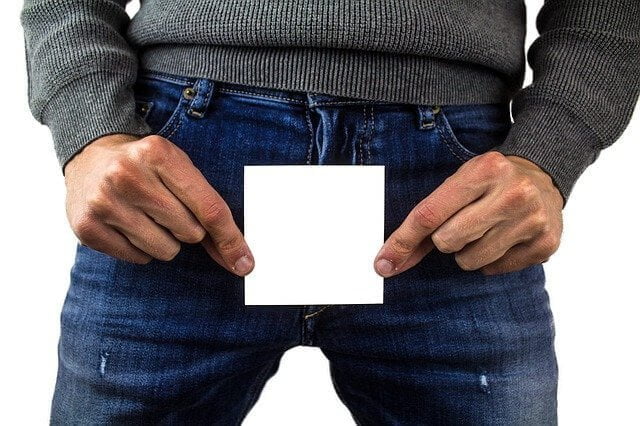
Breast Frame
The breast frame is the diameter around your chest just below your breasts. Using a tape measure, measure around your ribcage directly under your breasts. With the measurement, numbers add 5 to it. For example, if your frame measured 26 inches, when you add 5 to this you get 31 inches. You should round up to the nearest even number which is 32 inches. And since bras only come in even numbers, this will be your bra size, 32 inches!
Breast Size
The next measurement you need to take with the tape is breast size. Go around the chest over and include the fullest part of your bust (usually at the level of the nipples). This is the diameter of your chest plus your breast.
Breast Cup
To obtain the breast cup size, simply subtract Breast Frame from Breast Size (breast size – breast frame = breast cup).
The Bra Element
Is your bra the right size for you?
Besides support from mature nature, we also need material support for our breasts against the force of gravity. Over 80% of women do not know they are wearing the wrong size bra. Either too tight or too loose, too high or low, wrong cup size or old comfortable bras but doesn’t support breast, and so on. Our bust size changes with age, time, and weight fluctuations. Once in a while, we should also follow up with our measurements. If you are not sure, do not worry. Just visit the lingerie department and ask for sales assistance. Most big malls have friendly salesgirls to offer advice.
Are you wearing the bra correctly?
Tell signs that your bra is not right for you:
- Your breasts are drooping or looking generally out of shape when you put on the bra.
- Breasts pushed over the top of the cup.
- Red marks on your shoulders, breasts, or back caused by your ill-fitted bra or bra straps.
- The Center of your bra does not touch the breastbone.
- Any or all of these signs could tell that you are wearing the wrong bra size and that’s not only uncomfortable. Over time, it may distort the shape of your breasts and cause a variety of health problems, from headaches to backaches and even migraines.
Did you put on a bra correctly?
This may seem silly to women who have been putting on bras for years but there is indeed a proper way to do it. We recommend that you try the following steps when putting on your bra:
Slip your hands through the bra straps over your shoulders, lean and bend forward from the waist to allow your breasts to fall into the cups of the bra. Then, fasten the hooks of the bra.
While still in bending position, with one hand holding the side of the bra, insert the other hand in between the breast and the bra cup and push/scoop the excess flesh from the underarm area up and into the breast cup. Repeat on the other side. Stand up and make sure the breasts snug comfortably into the bra cups.
Next, looked into the mirror and see if the nipples are in the center seams of the bra cups if the front under bra band and the back band are at the same level (between the armpit and elbow). Lift your arms up. A well-fitted bra should not move around when you make any movement.
You can experiment with this method with your normal way of putting on a bra. You can really see the difference it makes.
You should also check on:
- The back of your bra does not ride up, otherwise, the under band may be too big, and you could need a smaller size.
- Your bra straps are not falling down or digging into your shoulders. If they are, adjust them or use wider straps.
- Your flesh does not squeeze over the top of your bra. If it does but feels fine everywhere else, the cup size is too small for you.
- Run your finger under the bra stripe in front. Your bra should be comfortable but not tight, otherwise, you need a larger band size or you must fasten your bra at the next looser hook.
- No, holes at the center of the bra and breasts. The middle of your bra lies as flat as possible against your breastbone for a comfortable fit.
Cup Size
Small breast, to make the most of a small breast, wears a soft or thin padded bra. This can give you an enhanced neckline, good uplift, and a lovely shape. Half-cup bras are also flattering for smaller busts, padding at the sides and under give a maximum lift to the breast, revealing sexy cleavages. Less endowed women should try to avoid bras that have square-cut, they only flatten your breast.
Big breasts or women with larger busts can get support from a bra with wider shoulder and back straps. Bras with full cups contain the breast better and give the breast a better appearance. Underwired bras provide better support under the bust while smooth, plain bra styles, without too much lace, help to make your bust appear smaller.
Different bra for different age
Breast sizes are growing in recent years as more women are having proper diet and breast supplements are the culprits. Bra-wearers are getting younger and larger too.
A child as young as 9 years old starts puberty. Significantly is her breast growth. Bra experts normally recommend cotton or thinly padded bra for young bra wearers as their breast development changes quickly and a soft bra allows breast tissues to stretch. For a mature female, a good comfortable bra to keep breasts in shape and support should be worn. Examples a sports bra, underwired bras, or padded bras.
Is it good to be braless?
Almost three-quarters of the day, a woman had her bra on. The good time for the breast’s skin to breathe and the breasts to rest is during bedtime. It is also a time for the breasts tissues to be fully relaxed. By going braless allows unrestricted blood circulation as well.